
Researchers at Texas Biomedical Research Institute are zeroing in on a new way to target tuberculosis (TB) infection. The National Institutes of Health (NIH) has awarded a four-year, $2.8 million grant for scientists to study the role of lung macrophages (immune cells) in metabolic and inflammation responses to TB. Findings could open the door to a new set of biological pathways critical to the body’s response to TB infection in the lungs.
“This newest research has the most clear-cut translation potential in terms of leading to a new strategy for host-directed therapy for TB,” said Texas Biomed President/CEO and Professor Larry Schlesinger, M.D., who is Principal Investigator of the study. “I think our discoveries could lead to a new set of drugs that will ultimately cure TB.”
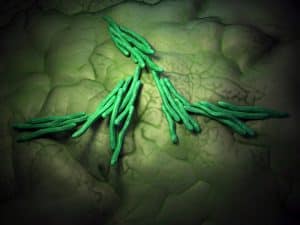
TB is a bacterial infection caused by Mycobacterium tuberculosis (Mtb). Still considered a modern day scourge, TB is the number one infectious disease killer in the world, claiming 1.3 million lives around the globe each year. It is primarily a lung disease spread when an infected person coughs out bacteria that are inhaled by someone in close proximity.
Antibiotic therapy for tuberculosis is long, toxic and not always effective. Many strains of the bacteria have developed drug resistance, creating challenges for physicians prescribing conventional therapies.
“I’m particularly interested in the concept of host-directed therapy,” Schlesinger explained. “It is akin to cancer immunotherapy. In both cases, we are now looking to bolster our body’s immune system to work in conjunction with antibiotics that treat the bacteria in order to eradicate the organism.”
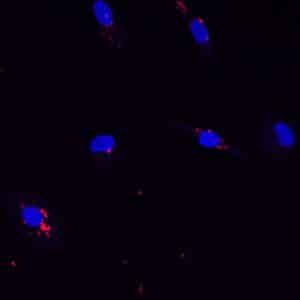
Dr. Schlesinger is a physician-scientist who focuses on the human immune system. The work horses of his research are immune cells called macrophages that live in lung tissue. Two types of macrophages are under study for this grant. One is derived from blood samples from healthy donors. The other cells are gathered from volunteers who undergo bronchoalveolar lavage, a medical procedure in which a bronchoscope is passed through the mouth or nose into the lungs and fluid is squirted into a small part of the lung and then collected for examination. Texas Biomed researchers are collaborating with Jay Peters, M.D., and his team, of the Pulmonary and Critical Care Medicine Division at UT Health San Antonio to collect these samples.
The ultimate goal of this research is to find out whether early events between Mtb and lung macrophages can predict host susceptibility or resistance to TB. Combining antibiotics with some kind of immune booster could lead to better outcomes by harnessing the body’s own power and leveraging it to target Mtb.
Macrophages in the lung are involved in metabolism of sugar and fat and regulation of inflammation. Dr. Schlesinger’s team is concentrating on proteins that are called nuclear receptors which regulate sets of genes in the nucleus of the macrophage. The team has identified a subset of these nuclear receptors that are very active in the lung. They hypothesize these are the master regulators of macrophage metabolism and inflammation and could be effective targets for new host-directed therapies.
One prototype protein under study is PPARg. This protein is already a target of a class of drugs called glitazones which help lower insulin resistance in type 2 diabetics. Dr. Schlesinger said if it is already a viable drug target for one disease, PPARg and similar proteins may make a good target for new TB drugs.
Schlesinger’s team is already testing come compounds in mice. Compounds with a positive impact will subsequently be tested in nonhuman primates at the Southwest National Primate Research Center on the Texas Biomed campus.
This research is funded by a grant from the National Institute of Allergy and Infectious Diseases (NIAID) of the National Institutes of Health (NIH) under award number AI136831. Texas Biomed Staff Scientist Eusondia Arnett, Ph.D., is also part of the team conducting the research.